20 The Half-Time Summary; What Have We Learnt, And What Solutions Are Outstanding?
In the introduction, I introduced 5 key themes to enable a Drug Development for Patients approach to drug development.
1) Understanding the goal
2) Understanding the science
3) Understanding dose-response models/modelling
4) Changes needed within the regulatory agencies
5) Changes needed within the pharmaceutical industry
Firstly, I covered why Patients Outcomes Must Come First. Here I motivated the need for personalised dosing, and explained what this meant. When we put individual patients outcomes first, the 3 steps we seek to understand in drug development are:
Given a patient’s individual characteristics, what is the best initial drug and dosing regimen?
If/when the initial dosing regimen needs to be changed for efficacy and/or safety/tolerability, how best to do this; what is the best science-based dose titration algorithm? That is, based on clinical endpoints, biomarkers, imaging and/or patient reported outcomes (PROs), when should the dose be changed, and by how much.
Under what circumstances should the dosing regimen be halted?
This set out our goal – getting the best outcomes for each and every patient by adapting (personalising) their dose.
I then gave a short review of the history of the design and analysis of RCTs. This covered what was good (e.g. randomisation, blinding, control groups), but then explained why we need to move beyond “agricultural” experimental design based on average patient outcomes to one where we refocus RCTs on individual patient outcomes; remember, patients are not fields! A brief history and overview of current “dose-ranging” trials was discussed, explaining how ICH E4 has wrongly led to simple, fixed-dose designs being favoured over more informative dose individualisation designs. Some modern D-R trials were reviewed, and shown to be very weak in terms of their design and analysis for both efficacy and safety/tolerability. These chapters served to provide the necessary context to explain the interrelationship between three choices/directions for drug development:
Individual patient outcomes versus Population (average) patient outcomes
Individual D-E-R relationships versus Population D-E-R relationships
The right designs and analyses of RCT to investigate the above and support drug approval.
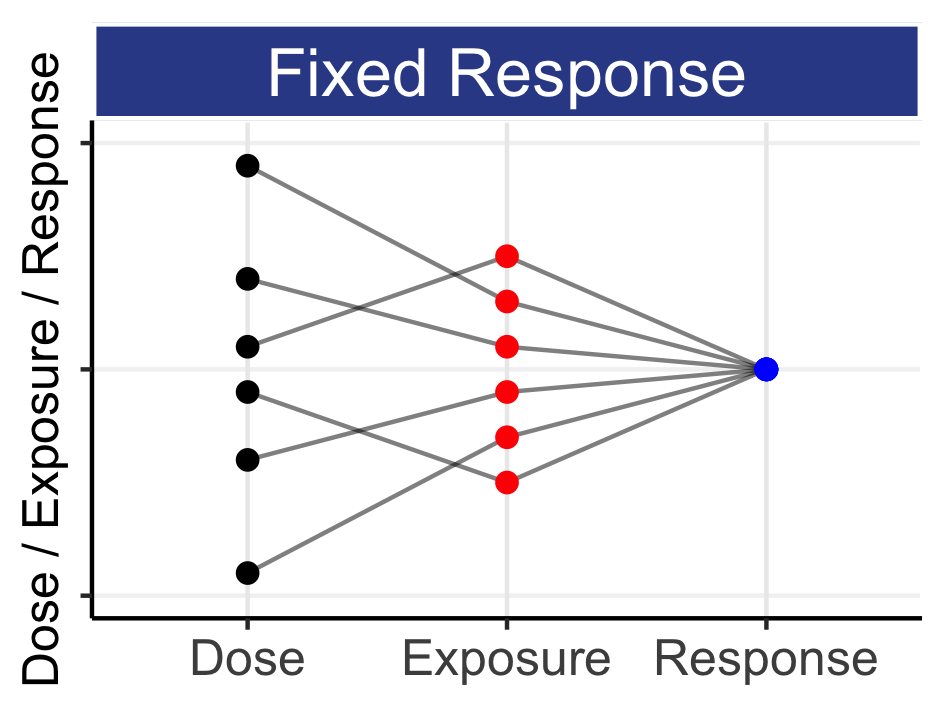
Historically we have relied on Population (average) patient outcomes from fixed-dose regimens because such a strategy is very simple. Unfortunately such a basic strategy does not achieve our goal; we do not get the best outcomes for individual patients.
The science of patient heterogeneity was then covered. This explained how IIV in PK and PD are the drivers of why patients need different doses, and how dose is just a very crude mechanism by which we seek to deliver sufficient drug to the site of action to illicit the desired PD responses in a patient. From anaesthetic agents to alcohol, we are all aware how different people need different “doses”; for most drugs, only dose individualised can deliver the best outcomes for each and every patient. We also viewed personalised dosing more from the patients perspective, and how they should be able to make decisions around their dose with consideration to their treatment goals, outcomes and personal preferences. As drug developers/regulators, we should ensure all approved dose ranges are scientifically justified, but we cannot tell people how they should feel.
To understand D-E-R relationships, we must use D-E-R models. The effects at different doses are always related to each, and suitable D-E-R models, such as the excellent sigmoidal Emax model, provide the best mechanism to allow us to “link” the effects across the different doses. Since the shape of D-E-R relationships are often poorly understood, I explained what “flat”, “typical” and “steep” D-E-R relationships look like for most clinical endpoints we encounter in drug development. Integrated D-E-R modelling across all doses/data is right, whilst “cherry picking” the observed outcomes at individual dose levels was shown to be unscientific and wrong.
The crucial differences between Population (average) and Individual D-E-R relationships were investigated further, explaining how the quantification of the Population D-E-R does not tell us about the shape of Individual D-E-R relationships. Where possible, we should always aim to understand individual D-E-R relationships, and fully acknowledge that each individual will follow their own D-E-R curve with increasing dose. Individual optimal doses are markedly different to any Population optimal dose. Like there is no single “optimal” dose across all patients, there is also no single therapeutic window and no single MTD. Many patients suffer terribly at “the” Population MTD, because this dose is much higher than their own MTD (MTDi).
In summary, the science tells us we need to consider Personalised Dosing for each patient. Unfortunately the same simple fixed-dose regimens for all patients will inevitably lead to poor outcomes for many patients; we can and must do better.
As our understanding of science, pathophysiology and clinical pharmacology has evolved, so must the remit and responsibilities of our regulators. To serve patients and society best we need, and must fund, Scientific Regulators. I explained how a Scientific Regulator must determine whether the drug is going to be used in a way that is best for patients; they will demand to see the accurate and precise quantification of Population and/or Individual D-E-R relationships for efficacy, tolerability and safety endpoints. A Scientific Regulator will advocate that such evidence is infinitely superior to simple “by trial, by dose” tables, listings, and P values. We cannot continue to accept Net Benefit regulators being compelled to approve drug regimens based on a (marginally) favourable benefit-risk assessment when there is little or no justification for the proposed dosing regimen; poor dosing choices by a pharmaceutical company directly leads to preventable harms to patients, and regulators should no longer tolerate this lack of scientific rigour. If we care about individual patient outcomes, we need Scientific Regulators.
Two regulatory pathways to approval were described, one based on Population outcomes (Approval P) and one based on Individual outcomes (Approval I). Approval P would be based on simple, fixed-dose, trial designs that use Population (average) patient outcomes for both benefits and harms. Approval I would be based on advanced trial designs where science-based dose titration algorithms are used to optimise the best Individual patient outcomes. Approval I will lead to Personalised Dosing and much better patient outcomes (our goal!), and the pharmaceutical industry can be encouraged to invest in the right trials to seek Approval I if, for example, it conferred a 5-year patent extension.
Two drug development strategies were introduced. Strategy I uses Individual outcomes to obtain Approval I for a smart science-based dose titration algorithm. It was shown how any dose titration algorithm to support Approval I would still produce tabular output for benefits and harms that is directly comparable to fixed-dose regimens. All stakeholders (regulators, patients, physicians, payers and the drug company) will help define what endpoints are important and work with analysts (like me) to design appropriate science-based dose titration algorithms. Strategy P uses Population outcomes to obtain Approval P for either Fixed-Doses (i.e. 1-2 doses) or a Hybrid dosing option, where a dose range in approved, with personalised dosing enabled via a simple dose titration algorithm. Strategy P is a simple drug development strategy, as it only requires a wide range of fixed-dose regimens to be studied throughout the whole drug development program.
The pharmaceutical industry also needs to carefully consider how Strategy I and Strategy P will deliver reimbursement and revenue. I discussed how modern value/outcome based pricing models are rightly aligning reimbursement with individual patient outcomes; individual patient outcomes are both the present and the future of reimbursement. The pharmaceutical industry must therefore embrace the challenge of employing Personalised Dosing to achieve the best outcome for each and every patient; it is what both patients and payers want, and it is therefore in their commercial interests to produce a wide range of doses to enable each patient to find the dose that works best for them. Do this, and companies will maximise their chance of having a happy “customer” and a continued revenue source (Insulin glargine (brand name Lantus) yielded >$70 billion in lifetime sales because it did this very well). The benefits of a subscription based pricing model for drugs was also introduced, whereby reimbursement is fixed whilst the patient remains (happily) on the drug (i.e. pricing is independent of the dose). I also discussed how both the pharmaceutical industry and regulators should utilise modern technologies to deliver a much better product to the “user”, the physician/patient. Current drug labels are verbose and not user friendly. In addition, post approval data that records patient engagement, adherence and PROs could, with permission, be collected across willing patients to enable multiple stakeholders (regulators, patient advocacy groups, payers) to further learn how different dosing regimens perform in a real world setting.
Finally, I introduced the value of using adaptive randomisation to most efficiently and ethically determining Population D-E-R relationships. This “learn as we go” approach starts with a randomisation schedule that supports a very wide dose range, and then “zeros in” on the optimal (most informative) doses based on updates to the randomisation allocations determined by a DMC. Adaptive randomisation is most valuable when our initial assumptions about the location and shape of the D-E-R relationships are imperfect. The ASTIN and AWARD-5 trials are two excellent examples that successfully employed adaptive randomisation; however the general scarcity of such trials for D-E-R trials would suggest the considerable advantages of these trials is currently not well understood. These adaptive trial designs can most quickly and cheaply quantify D-E-R relationships for both efficacy and safety, and hence should be a central component of any modern drug development program.
At this stage, I hope you are convinced of the “why” – the science tells us that we must seek to understand Population and Individual D-E-R relationships, and why we must always consider Personalised Dosing. Some of the “how” has also been addressed, including the general strategies to obtain Approval P based on Population (average) patient outcomes and Approval I based on individual patient outcomes.
What remains is the technical roadmap for the drug program and supporting trial designs; what does a company wishing to pursue Approval P and/or Approval I need to do, and how should the regulators work with them to ensure the evidence base for approval is as strong as it can be. These are the topics of the remainder of this book (in short, there are no technical barriers…we know how to do it!)