17 Changing How We Pay For Drugs; Value/Outcome-Based Pricing And Subscription-Based Pricing
At the end of this chapter, the reader will understand:
That expecting reimbursement/payment for a drug for a particular patient based on “average” outcomes in other patients is odd.
What is value/outcome-based pricing, and how it should refocus drug manufacturers to use personalised dosing to achieve the best outcome for each and every patient.
It is in the drug manufacturers commercial interests to produce a wide dose range to enable each patient to find the dose that works best for them; otherwise they lose the patient, and further revenues, forever.
For some indications/drugs, it would be more sensible to employ a subscription-based pricing, whereby the drug manufacturer is paid whilst the patient is (happily) using the drug (i.e. the subscription price is independent of the dose/usage).
When it comes to how we pay for drugs, consider this analogy. Imagine that you buy a new TV. When you plug in the TV, you get an awful picture. You call the manufacturer, and they take your personal details. They respond “Well, that is interesting. According to our data, we have many people like you who did achieve an acceptable picture”. This would be a comical interaction; as a consumer, I have no interest in whether a product worked for “people like me” or works “on average”; I would be very unhappy with the product, and demand my money back. I hope this analogy brings into sharp focus the inherent shoddiness in how drug manufacturers often expect to be reimbursed/paid for their products. I cannot think of another industry that expects full payment when their product fails to deliver. The introduction of value/outcome-based pricing will rightly bring much greater scrutiny to individual patient outcomes.
Value/outcome based pricing is where the reimbursement for the drug is directly linked to the value/outcome achieved for the patient.
In the most basic sense, if the drug fails to deliver real benefits for the patient, the manufacturer does not get paid. An excellent and fair system!
I view the emergence of value/outcome-based pricing as a “game changer” in how the pharmaceutical industry must approach dosing, and the central role of personalised dosing. The industry has a choice. Either develop a “one-size-fits-all” dose based on “average outcomes” that is poorly aligned with value/outcome-based pricing, or develop a smart dose-titration algorithm (with a wide range of potential doses available to each patient) aimed at maximising individual patient outcomes that is fully aligned with value/outcome-based pricing.
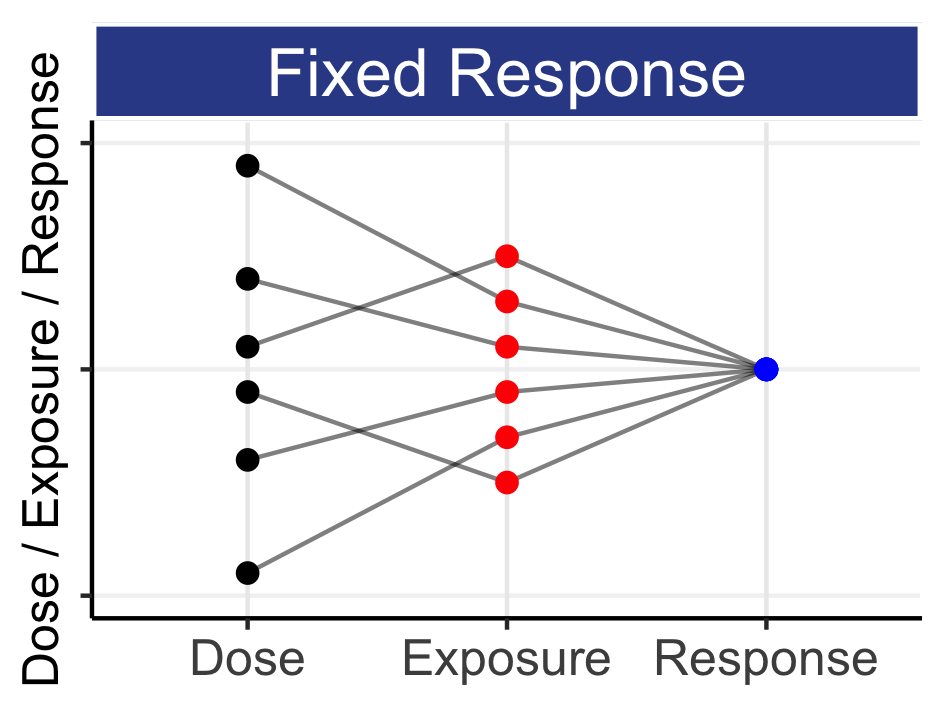
add a graph showing a range of outcomes based on fixed-dose regimen, and the higher range with individualised?
From a purely commercial perspective, it is clear that offering multiple dose levels will enable multiple opportunities to achieve success for the patient, and hence the greatest chance of continued reimbursement.
Having multiple doses will require additional manufacturing requirements and devices such as the injection pens used so successfully with insulin glargine, but this “cost” will be minor relative to the overall cost of the drug, and the value that it brings to both the patient and the manufacturer (longer patient usage). In short, companies need to prospectively develop and utilise commercial products/devices that support a very wide range of dose levels (=support personalised dosing).
Unfortunately not every therapeutic area will have a clear, objective measure of value. For example, whilst a type 2 diabetes drug could be reimbursed relative to the magnitude of the improvement in glucose control (e.g. the % reduction in HbA1c), for an oncology drug the primary endpoint could be the overall survival of the patient. Although alternative measures of value could exist (e.g. reduction in tumour size), we can consider alternative reimburse models that fully enable personalised dosing.
We can reimburse drugs based on a subscription-based pricing model.
The streaming services provided by Netflix and Spotify require the user to pay a fixed price for access to the service, and therefore the price paid is independent of usage. Similarly my daughter pays a monthly fee to the opticians for monthly contact lenses and yearly check-ups. It is in the interest of my daughter, the optician and the manufacturer to ensure her needs are continually met every year. In particular, if her prescription changing over time, the cost remains the same (the manufacturer has developed/planned to support a wide range of prescription strengths). For some drugs/indications, we could apply a similar subscription-based pricing model. The reimbursement would not be linked to the actual dose, but rather on having access to the drug (i.e. the price paid is independent of the dose). Whilst the patient uses the drug, the company is paid. The beauty of these relationships is that all parties benefit when the patient receives the best dose, and hence outcomes, for them.