15 The Two Regulatory Approval Pathways; “Approval P” and “Approval I”
At the end of this chapter, the reader will understand:
The need for clearly defined regulatory pathways based on Population outcomes (Approval P) and/or Individual outcomes (Approval I)
How Approval P is based on simple, fixed-dose, parallel group, trial designs that use Population (average) outcomes for both benefits and harms. Such trials are not aligned with outcome/value based pricing.
How Approval I is based on advanced trial designs where science-based dose titration algorithms are used to optimise the best Individual patient outcomes. Such trials are aligned with outcome/value based pricing.
How Approval I will lead to Personalised Dosing and better patient outcomes, and can be stimulated if Approval I resulted in a 5-year patent extension.
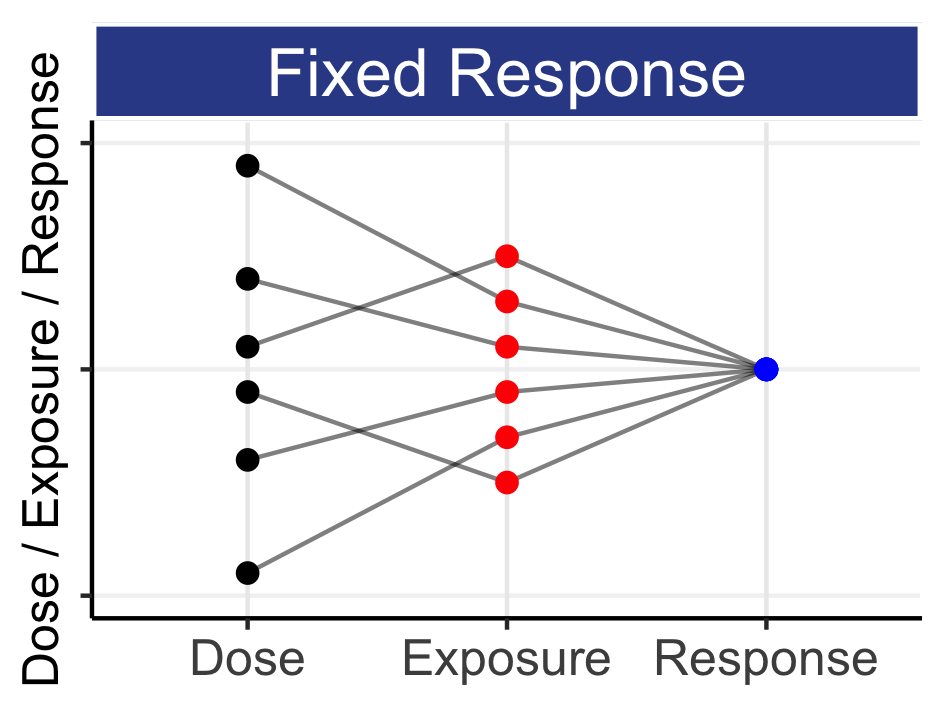
It has been argued that we must look to understand the dose response at both the Population and Individual levels if we are to truly understand how best to use a drug, and that we need both the sponsor to conduct the right trials/analysis, and a Scientific Regulator to work with the sponsor to ensure that the drug dosing regimen algorithm is the best that it can be.
At a recent FDA-ASCO meeting discussing dose optimisation, an industry representation cautioned against raising the bar for approval with the requirement to actually understand the D-E-R relationship at approval. Indeed, such an argument can be augmented by stating that the requirement for such information would delay access to badly needed drugs with novel mechanisms of action in areas of high unmet need. Overall, I do not find these arguments fully compelling, but clearly the right trials may require additional time, cost and expertise for both sponsors and regulators alike.
We can hope for change, but I am sceptical that without a clear distinction between drug development approval based on Population and Individual outcomes, Drug Development For Patients and Personalised Dosing will not gain the traction that we need. We need a clear pathway for each; a proposed solution is shown in the Table 15.1.
| Criteria | Approval P (Population) | Approval I (Individual) |
|---|---|---|
| Trial Designs | Simple | Simple / Advanced |
| Dosing Regimens Studied | Fixed Doses | Many / Titrated Doses |
| Patient Population | Narrow or Wide | Wide |
| Target Outcome Measures | Population/Average Outcomes | Individual Patient Outcomes |
| Regulatory Review | Net-Benefit | Scientific |
| Drug Label Dose | Fixed dose | Dose titration algorithm |
| Personalised Dosing | No | Yes |
| Fully Aligned with Outcome/Value Based Pricing | No | Yes |
| Patent Exclusivity | Standard | Standard + 5 years |
Most current drug development programs seek Approval P, where the focus is typically on simple designs that look at Population outcomes in 1-2 key fixed doses, often in a narrow patient population (i.e. with many exclusion criteria used in the randomised clinical trials). Based on efficacy and safety summaries with Population outcomes, a Net-Benefit Regulator can consider whether the proposed dose regimen(s) is/are, on balance, favourable. Under this pathway, the dosing regimen is neither optimised at either the Population or Individual level, nor aligned with outcome based pricing. As such, although scientifically limited, it can be reasonable for the regimen to achieve Approval P. This would allow early access to the drug, albeit with a dosing regimen that is not optimised in any way.
The table also shows Approval I, where the focus has shifted to individual patient outcomes. The trial designs will typically be more complex, and the focus will be on finding the best science-based dose titration algorithm to enable Personalised Dosing. The trials may also consider a more diverse/representative patient population (i.e. fewer exclusion criteria), and use more patient specific outcomes (e.g. PROs) that are fully aligned with outcome/value based pricing measures.
Whilst I believe only Approval I ensures personalised dosing for both current and future generations of patients, the dual pathways above provide a framework whereby we can transition smoothly from the Population system based on fixed doses and Population outcomes to the Individual system that targets finding the right dose for each patient as efficiently and quickly as possible using an intelligent dosing algorithm.
Approval I should include multiple stakeholders who currently may not interact as fully as we would hope. For example, imagine designing the trial with payers and patient advocacy groups in the same room as the sponsor and regulators. Could they agree on a trial design that works for all? Fundamentally, everyone wants the same thing; the best outcomes for each patient, thus I am optimist that acceptable solutions could would be found.
To make Approval I happen, we need to create a “win-win” environment for all. This is where a patent extension must come in. If the sponsor does achieve Approval I, a 5-year extension to the patent exclusivity would be granted. This “reward” for the sponsor would encourage them to invest in the right trials to seek Approval I. Their submission fees would help fund additional resources needed by the regulators to assess the scientific integrity of these dose individualisation trials. Both current and future generations of patients (and society in general) would benefit from improved individual outcomes from intelligent, science based, dose titration algorithms, and payers would have the right data to agree reimbursement with sponsors based on value/outcome based pricing.
If Approval I were available tomorrow, we would see innovation in exactly the areas we would desire. For example, some sponsors would see the opportunity to extend the revenue cycle of their commercially successful drugs. Although driven my financial motives, the outcome here would still be very positive. These drugs are (demonstrable) good, but we would have the opportunity to gather much better data to truly maximise their benefits via personalised dosing; we would be turning good drugs into great drugs for both current and all future generations of patients (experienced drug developers could point to a wide range of drugs that are frequently prescribed for decades, but with poorly justified dosing regimens with little/no quantitative advice on how to “tailor” the dose based on accruing efficacy/safety data for a patient)).
In areas of high unmet need, such as rare diseases, sponsors would see the importance of immediately building in dose modifications for each and every patient, in pursuit of the best outcomes for each and every patient. Initial dose selection, followed by (intelligent) dose titration follows immediately when we seek to maximise the outcome of “this” patient. Conversely, I have seen trial designs for rare indications that are simply fixed-dose phase 3 type trials but in very few patients. These sponsors seem paralysed by the apparent need for a standard Approval P program, but the resulting trial data serves no one. Particularly in rare diseases, trying to find the “one-size-fits-all” dose makes absolutely no scientific or ethical sense. The opportunity to seek Approval I (and not Approval P) would enable these sponsors to fully focus on maximising individual patient outcomes, as both patients and regulators would wish.
It could be argued that this “win-win” approach has a loser - the payer in the extended 5-year period. However I would argue we are (collectively) paying $1 to get, say, $5 in return. The application of Personalised Dosing will benefit patients/payers both before and (long) after the 5-year period. Costs, such as hospital admissions and absence from work, will be reduced when we get the dosing right. Patients will be better treated, and be happier. The benefits to society will extend indefinitely.
In summary, the complementary pathways of Approval P and Approval I precisely clarifies the distinction between population and individual based outcomes, with Approval I leading to a modern drug development paradigm that uses Personalised Dosing to achieve the best outcomes for each and every patient.